Our beloved father and husband, Peter Klassen, age 77, of Steinbach, Manitoba, passed away suddenly on Thursday, October 17, 2024, at his home surrounded by his devoted family.
Peter is survived by his loving wife Luella Klassen of 57 years, his son Prescott Klassen, his daughter Natasha Klassen, his only grandchild Benjamin Wiebe. He is also lovingly remembered by his daughter-in-law Monica Lisafeld, his son-in-law Michael Major, his siblings, and many dear friends.
Peter was predeceased by his parents Nettie & Cornelius (C.U.) Klassen, his sisters Leona, Sandra, Lisa, brother Bernie, sister-in-law Roxanne and his in-laws Bennie D & Helen Reimer and his brother-in-law Eric Bragg.
Peter, or Peitatji, as he was fondly known by many, was a man who went out into the world to embrace everyone he met with a spirit of love and friendship. He was an exceptional father, Papa and husband. He loved his family with every fiber, as well as the Lord. Peter spent his life helping others and his unconditional acceptance of others will be remembered by the many he “adopted” as family.
He will be dearly missed by many in the community of Steinbach and surrounding area due to his many efforts to help others and his amazing talent of connecting with the people he met. Peter could speak with anyone and would go out of his way to create a welcoming environment for all he encountered. He also owned and operated Klassen Computer Connections for two decades and served the Hanover area with the most genuine and exceptional service. Peter brought his love of the Lord and his love of others into everything he did, this was seen in his business practices and his daily interactions with the many people he met every day.
Peter spoke several languages, he loved words, knowledge, history, science, birds, animals, the exploration of space, discussions of topics that explored many ideas and creativity. He will be deeply missed by his family and friends.
If friends so desire in lieu of flowers, Peter would have appreciated donations made to charities that support children and mental health.
We as a family would like to send our deepest gratitude and thanks to the men and women of the emergency services; the RCMP, the Fire Department, the Paramedics and the Bethesda Emergency staff who all were so compassionate and helpful.
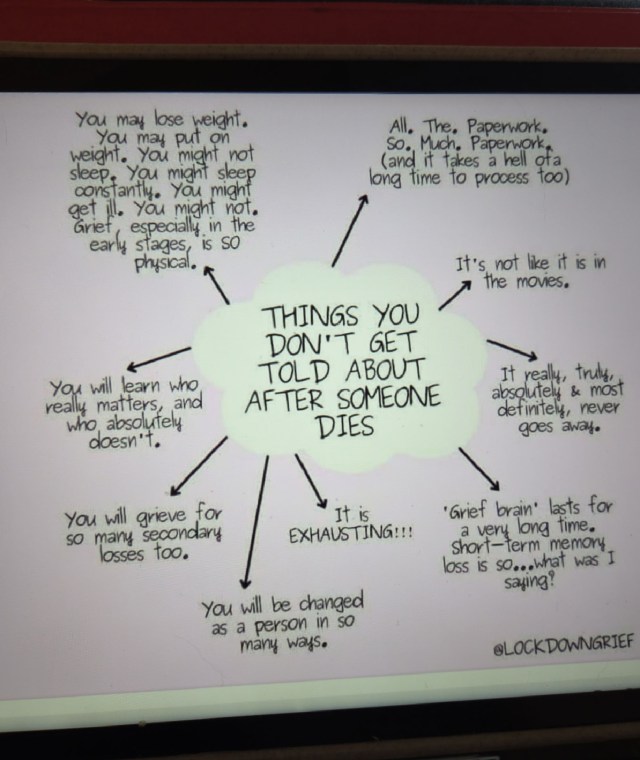


 t has been 8 1/2 months since my husband passed away. During this time, I have experienced loneliness, sadness, anger, and depression. I had no idea how difficult it would be to work through all the paperwork left for me to deal with. In this post, I have included some of the things I learned while working through this nightmare called widowhood.
t has been 8 1/2 months since my husband passed away. During this time, I have experienced loneliness, sadness, anger, and depression. I had no idea how difficult it would be to work through all the paperwork left for me to deal with. In this post, I have included some of the things I learned while working through this nightmare called widowhood. «Христос Воскрес» is the Ukrainian Easter greeting, and means “Christ has risen.” During Easter service (which, for the orthodox, is a midnight mass), the priest shouts this to the congregation, who answer «В
«Христос Воскрес» is the Ukrainian Easter greeting, and means “Christ has risen.” During Easter service (which, for the orthodox, is a midnight mass), the priest shouts this to the congregation, who answer «В
 October and November have been lonely and difficult. My husband, Peter, of 57 years, passed away suddenly without warning during the evening of October 17th. When it became obvious that he needed medical intervention, even though he was adamant about not calling 911, I did just that. The emergency services arrived quickly and transported him to the hospital. Our grandson and I arrived at the hospital emergency department shortly after my husband. We were told his prognosis was not good. That was the first time I realized that he might die. Our grandson has a suite in our basement. He has been and continues to be a tremendous help and emotional support. My daughter and her partner arrived at the hospital after her father died. They spent the weekend with me and helped with arrangements at the Funeral Home. Our son arrived from Seattle a few days after his dad’s death and spent two weeks with me. He is coming back next week and plans to stay for 14 days. I do not know how people can plan a funeral or a memorial a few days after a sudden death. As a family and with the support of the funeral home staff, we decided to have a Memorial in the spring. According to the Cleveland Clinic, grief involves coping with loss. It’s important to remember that grief doesn’t fit into neat boxes or timelines. Everyone experiences grief in their own way. Also, there’s never a time when you’re “done” with grief. Your connection with a loved one who’s passed becomes integrated into your ongoing life story. It’s forever a part of who you are.
October and November have been lonely and difficult. My husband, Peter, of 57 years, passed away suddenly without warning during the evening of October 17th. When it became obvious that he needed medical intervention, even though he was adamant about not calling 911, I did just that. The emergency services arrived quickly and transported him to the hospital. Our grandson and I arrived at the hospital emergency department shortly after my husband. We were told his prognosis was not good. That was the first time I realized that he might die. Our grandson has a suite in our basement. He has been and continues to be a tremendous help and emotional support. My daughter and her partner arrived at the hospital after her father died. They spent the weekend with me and helped with arrangements at the Funeral Home. Our son arrived from Seattle a few days after his dad’s death and spent two weeks with me. He is coming back next week and plans to stay for 14 days. I do not know how people can plan a funeral or a memorial a few days after a sudden death. As a family and with the support of the funeral home staff, we decided to have a Memorial in the spring. According to the Cleveland Clinic, grief involves coping with loss. It’s important to remember that grief doesn’t fit into neat boxes or timelines. Everyone experiences grief in their own way. Also, there’s never a time when you’re “done” with grief. Your connection with a loved one who’s passed becomes integrated into your ongoing life story. It’s forever a part of who you are.